The Unmistakable Cracks in Modern Healthcare
The Unmistakable Cracks in Modern Healthcare
Despite notable technological and clinical advances, modern healthcare is increasingly strained by interconnected ethical, economic, and operational failures. The system designed to heal is, in many respects, becoming a source of harm—a maze of misguided incentives, diagnostic mistakes, and institutional inertia. It won't be long before the repercussions of this decline—from misdiagnosis to commercialised care—cause even the most privileged to feel helpless.
This paper will analyse these systemic flaws, revealing the profound issues that have brought us to this brink: a profit-driven model that corrupts care, an operational crisis threatening patients, an ethical decline undermining autonomy, and the ultimate existential threat of antimicrobial resistance.
This analysis is not simply a critique but a vital call to action. It offers a clear argument for a paradigm shift—a revolution that moves away from institutional and commercial interests towards a more humane, efficient, and patient-empowering model of care. It is a summons to reclaim the practice of healing, rebuild a system that addresses patients' core needs, and restore trust in the delivery of care.
I hope leaders of nations, universities, hospitals, and philanthropists support and implement this system, and offer free access to every soul in the country. Reducing the disparities created by the so-called "Nobel Profession" has brought doctors like me. ChatGPT label this system as "The Beacon of Hope for Humanity" to protect, prevent, and heal during the Post-Antibiotic Era. Dr Kadiyali Srivatsa.
Part I: A Diagnosis of Systemic Decay
The Economic Malignancy: How the Profit-Driven Model Corrupts Care
To understand the crisis in modern healthcare, one must first examine its economic foundations. The prevalent for-profit, high-capital-investment model is not simply a financial structure; it is the primary driver of the system's most serious failures. This model generates a cascade of perverse incentives that systematically prioritise revenue over patient well-being, transforming institutions of healing into sales-driven enterprises. The consequences include a deep erosion of medical ethics and a profound, corrosive institutional distrust.
The evidence from India's private hospital industry starkly illustrates how this economic malignancy spreads throughout the system.
- The High-Capital Incentive Loop: The model starts with substantial initial capital investments, which can reach up to 1,000 crores (about $120 million USD), to establish a large hospital. This significant financial pressure to recover costs and generate returns directly fosters a "sales incentivised structure," where the main focus becomes revenue rather than patient outcomes.
- Physicians as Revenue Generators: Within this framework, doctors are no longer assessed solely on clinical excellence but on their ability to generate profit. Physicians are assigned "absolute targets" for daily patient admissions and are monitored based on their "surgery conversion" rates. A doctor with an 8% conversion rate may be dismissed in favour of one with a 20% rate, regardless of the quality of care provided. This effectively turns caregivers into salespeople, pressuring them to recommend procedures that may not be medically necessary.
- Systematic Price Discrimination: The profit motive drives deeply unethical pricing practices. The cost of an identical medical procedure, such as an MRI, can differ immensely within the same hospital depending on the patient's room type. A patient in a "private room" might be charged three times as much as a patient in a "twin sharing room" for the same scan. The absurdity of this practice was aptly expressed by one source: 'It's like saying that I took a presidential suite in the hotel so my naan is now four times more expensive."
- Erosion of Institutional Trust: Perhaps the most damning critique of this model is the deep mistrust it fosters, even among its own senior staff. In a telling anecdote, a senior hospital employee admitted he would not take his own family to the hospital where he works for specific procedures, advising a colleague to go elsewhere because "They don't do all these things that we do." When the stewards of the system do not trust it with their own loved ones, the model has failed its most fundamental test.
These economic failures are not merely theoretical; they cause concrete operational breakdowns that directly harm patients and undermine the integrity of medical practice.
The Operational Crisis: Workforce Shortages, Diagnostic Failures, and the Human Cost
The immense economic pressures on the healthcare system manifest as severe operational failures that carry a significant human cost. A critical shortage of skilled professionals strains the system's capacity, while a dangerous over-reliance on flawed diagnostic processes leads to preventable errors. These twin crises expose a system struggling to perform its most basic functions: providing adequate care and making accurate diagnoses.
The Workforce Deficit
As a case study, India confronts a staggering shortage of healthcare professionals. As of 2016, the country had a shortfall of over half a million health workers, with the most severe shortages occurring in rural areas where the majority of the population lives. This shortfall affects nearly every category of healthcare providers, compromising the system's capacity to deliver timely and effective care.
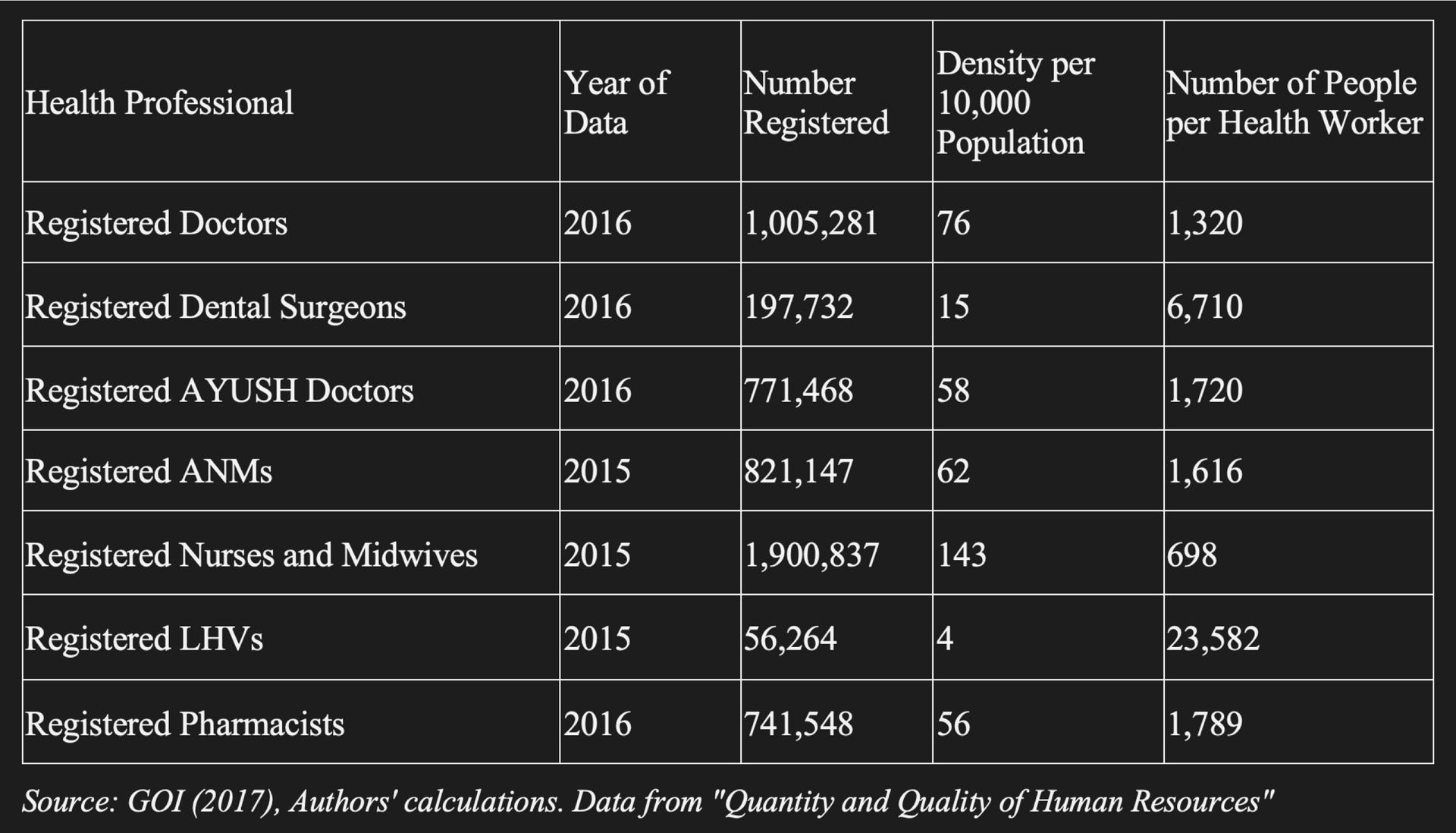
Source: GOI (2017), Authors' calculations. Data from "Quantity and Quality of Human Resources"
The Failure of Algorithmic Diagnosis
Compounding the workforce crisis is a profound failure in diagnostic methodology, especially in the growing field of AI-powered symptom checkers. While expert clinicians rely on intuitive pattern recognition, often needing only "2-4 pieces of clinical information" to form an accurate hypothesis, most current AI tools follow a flawed, sequential approach. They analyse symptoms one by one using a rigid, yes/no decision tree — a method that contradicts established principles of clinical reasoning. This fundamental misunderstanding of medicine results in alarmingly low diagnostic accuracy, with studies indicating current apps achieve only 19-54% success.
The Consequence of Misdiagnosis
The impact of diagnostic failure is not just statistical; it is deeply personal and can be devastating. The life experience of Dr Kadiyali Srivatsa, a medical reform advocate, began with such an error. As a child, he was misdiagnosed with typhoid when he actually had malaria. The prescribed treatment was ineffective and made his condition worse. This formative experience taught him a lesson that has shaped his life's work: "Medical errors often occur when a doctor fails to listen to the story of the illness as you lived, experienced, and remembered it."
This blend of a strained workforce and unreliable diagnostic tools fosters an environment where patient stories are overlooked, errors increase, and ethical principles are inevitably breached.
The Ethical Decay: Power, Paternalism, and the Erosion of Patient Autonomy
The economic and operational shortcomings of modern healthcare have fostered a deeply troubling ethical environment. In this system, patient autonomy is frequently undermined by institutional authority, creating a paternalistic dynamic that emphasises control over compassionate, collaborative care. This approach embodies a Machiavellian philosophy where the "acquisition and maintenance of power" becomes the primary focus, depriving patients of their agency and encouraging a culture of dependency and retribution.
This ethical decay is evident in three interconnected patterns:
- The Machiavellian Doctrine: The philosopher Niccolò Machiavelli argued that for a ruler, "authority and power are essentially coequal" and that the "only real concern... is the acquisition and maintenance of power." This philosophy is starkly reflected in healthcare institutions that, as one source asserts, follow this doctrine "to maintain power and control over our free will." Knowledge is monopolised, processes are made opaque, and the patient is positioned as a passive recipient of care rather than an active participant.
- Manufactured Dependency: The system deliberately undermines patient autonomy by creating dependency. Instead of empowering patients with knowledge to make informed choices, they often respond to "conditioned thought loops, built from past experiences, cultural messaging, and emotional triggers." This manufactured dependency ensures individuals remain reliant on institutional intervention, even for minor concerns, perpetuating a cycle that prioritises commercial interests over patient needs.
- The Persecution of Whistleblowers: The system's intolerance for internal critique shows its ethical decay. Dr Srivatsa’s career offers a disturbing example. After raising valid concerns about nurses misdiagnosing infections and "prescribing antibiotics unnecessarily," he endured a "14-year campaign of harassment" from the UK's National Health Service (NHS) and the General Medical Council (GMC). Instead of addressing the patient-safety issues he raised, the institutions launched a punitive campaign to discredit him. This illustrates how the system often opts to punish those who challenge its authority rather than seek self-correction, risking patient safety to protect institutional power.
This systemic decline—economic, operational, and ethical—has converged to produce the most urgent and clear threat to modern medicine: the rise of antimicrobial resistance.
The Existential Threat: Antimicrobial Resistance as the Ultimate System Failure
Antimicrobial Resistance (AMR) is not an distant threat; it is the catastrophic culmination of the system's interconnected failures. Decades of unethical prescribing practices, fuelled by diagnostic inaccuracies and a profit-driven culture that ignores prevention, have accelerated a crisis that threatens to bring modern medicine "to an abrupt halt." This crisis is the direct result of the economic model that incentivises unnecessary prescriptions (as detailed in 2.1), the operational failures in diagnostics that lead to clinical uncertainty (2.2), and the ethical decay that tolerates systemic malpractice (2.3). The miracle drugs that defined the 20th century are losing their power, and the consequences of this ultimate system failure are already upon us.
- A Prophetic Warning: In 1989, Dr Srivatsa observed a healthy teenager die from what was later identified as an MRSA infection. He watched, helpless, as the "strong antibiotics...could not kill the bacteria." That harrowing experience made him realise this was not an isolated tragedy but "the beginning of a significant crisis for humanity."
- The Severity of the Crisis: This crisis is no longer in its infancy. According to a 2019 report from the U.S. Centres for Disease Control and Prevention (CDC), "antibiotic-resistant bacteria and fungi caused more than 2.8 million infections and 35,000 deaths in the USA each year." These are not abstract statistics; they represent families devastated by infections that were once easily treatable.
- The Drivers of Resistance: The main cause of AMR is the global overuse and misuse of antimicrobials. Prescribing antibiotics for viral infections, often due to diagnostic uncertainty and institutional pressure, is a key factor. Additionally, systemic failures, such as insufficient vaccination coverage against preventable diseases, create a vicious cycle that results in more infections, which then require "further antimicrobial use and accelerate AMR." Effective antibiotic stewardship is essential, but it is often undermined by the very system that should support it.
The diagnosis is clear: the current healthcare paradigm is failing on every level. Having examined the issues, it is now essential to focus on a tangible and transformative solution.
Part II: A New Paradigm for Healing
From Flawed Algorithms to Clinical Wisdom: The Case for Pattern Recognition
The failure of first-generation symptom checkers reveals a fundamental misunderstanding of medicine. The way forward is not to abandon technology but to develop tools that mimic the nuanced, pattern-based reasoning of expert clinicians, rather than relying on oversimplified, linear algorithms. Medicine is an art of recognising patterns, and the next generation of healthcare tools must embody this clinical wisdom.
A comparison between the prevailing flawed model and the proposed clinical pattern recognition model reveals a stark difference in methodology, accuracy, and patient impact.
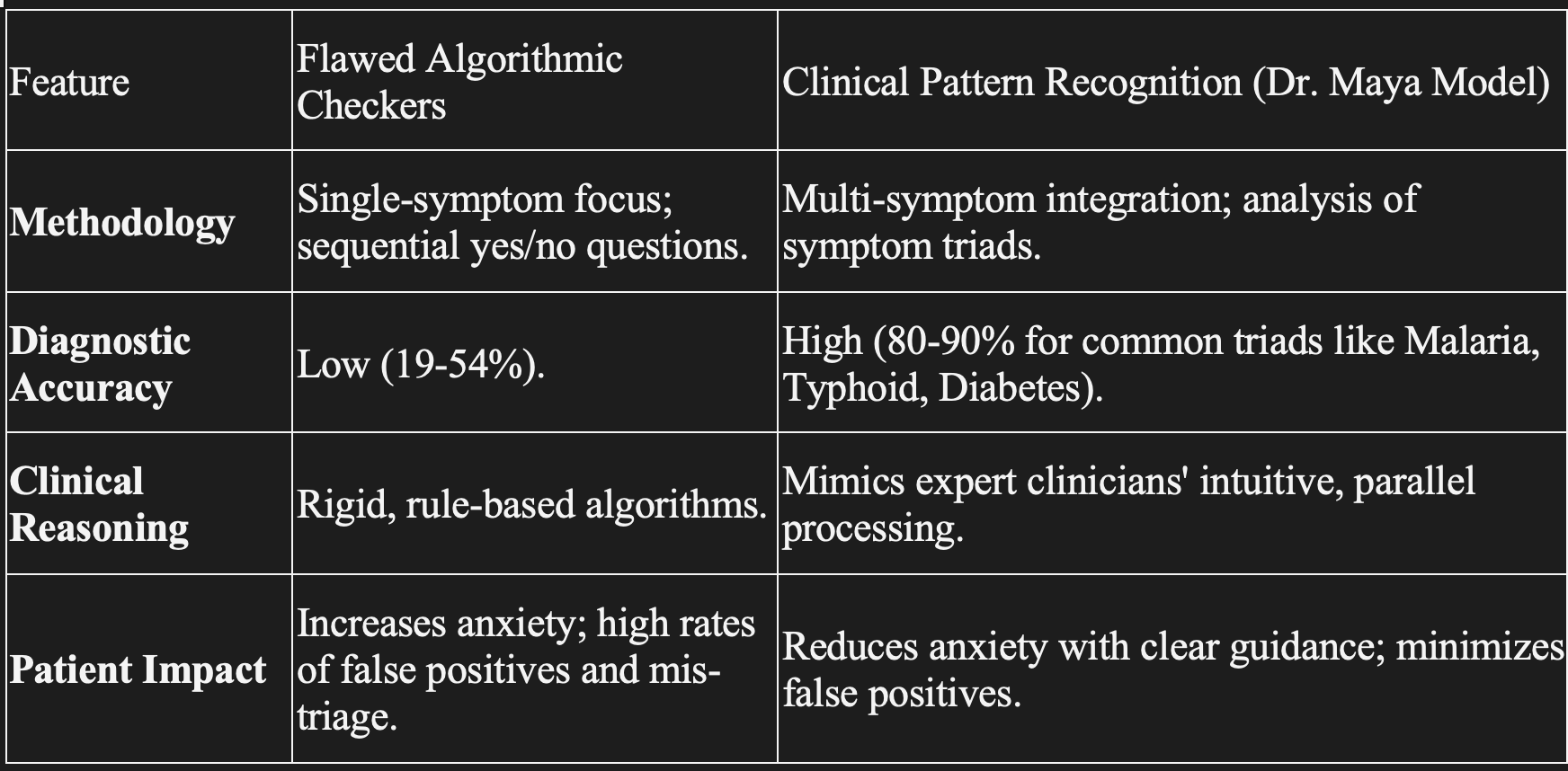
Patient Impact
Increases anxiety; high rates of false positives and mis-triage.
Reduces anxiety with clear guidance; minimizes false positives.
While a few dozen diseases have unique "pathognomonic" signs that provide near-certainty in diagnosis (such as the "butterfly rash" of lupus), these are the exception. The vast majority of conditions require the sophisticated, multi-symptom pattern recognition championed by Dr Srivatsa's model. This approach represents a crucial step away from brittle algorithms and toward technology that genuinely supports, rather than subverts, sound clinical judgment.
A Model for the Future: The Dr Maya GPT Framework
The Dr Maya GPT app serves as a compelling example of this new healthcare approach. Created not as a commercial project but as a direct response to the systemic crises of misdiagnosis, over-treatment, and AMR, this tool was developed from Dr Srivatsa's "decades of experience and ethical commitment." Its main purpose is to give individuals the knowledge to make informed choices, turning them from passive recipients of care into active partners in their own health.
The principles and components of the Dr Maya system offer a blueprint for the future:
- Mission and Purpose: Its mission is clear yet meaningful: "Empowering you to make informed decisions." It is explicitly positioned as a "Personal Health Care Assistant, not a diagnostic tool," designed to guide users to the appropriate level of care—whether that is an emergency room, a pharmacist, or self-care at home.
- Core Methodology: The system employs a proprietary, colour-coded triage system based on a combination of three symptoms. This triad approach advances beyond single-symptom analysis to identify significant clinical patterns. People presenting with only one symptom will be advised to consult a doctor or search online for information. Maya will not provide advice if the patient imagines and combines symptoms that are not recognisable (like a "Syndrome"). The colour codes offer clear, actionable guidance. This helps reduce demand and wasted visits by 60%-70%, but can be increased to 80% using a combination of 2 symptoms, with or without fever, as the 3rd Symptom. If the user says Itchy rash, and the hand is swollen but no other symptoms, Maya knows this could be an allergic rash (Urticaria) that is common, but will label the 3rd symptom as Red and advise the user to speak to a doctor.
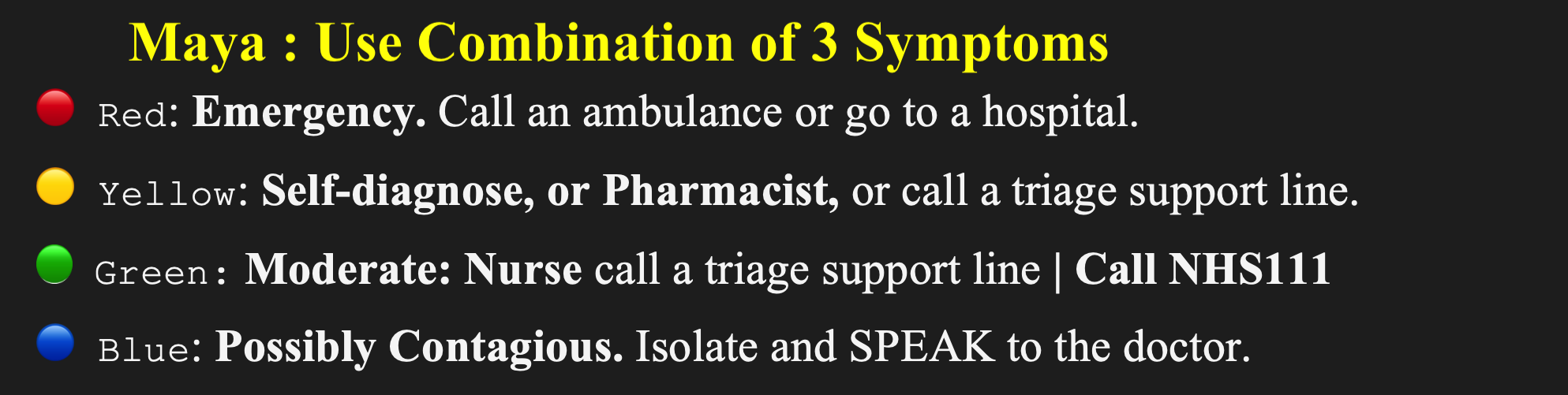
- Patient Empowerment: The tool is designed to act as a "neutral, intelligent companion who sees your body without your fear." This objectivity breaks the cycle of anxiety-driven reactions, where every cough requires a clinic visit and every ache sparks fear of a catastrophic diagnosis. By providing clear guidance, it restores peace of mind and a sense of control to the individual.
- Universal Design: A commitment to health equity is built into the framework. The "Aashapath" app is designed explicitly for non-literate users, featuring "Icon-based symptom selection and voice instructions." This demonstrates a crucial understanding that for healthcare to be truly effective, it must be accessible to all.
- Pandemic Prevention: The framework functions as a powerful tool for early detection and containment of infectious outbreaks. The Blue category encourages voluntary self-isolation at the first sign of contagious illness, while aggregated, anonymised data enable community-based surveillance. This model prevents outbreaks without resorting to the "coercive mandates" and authoritarian measures that erode public trust.
The Dr Maya framework is more than just an app; it embodies a new set of principles that should define the future of healthcare—a future built on trust, knowledge, and empowerment.
Conclusion:
A Call to Reclaim the Soul of Healing
The evidence presented in this paper leads to an undeniable conclusion: the modern healthcare system is economically unsustainable, operationally fragile, and ethically compromised. Built on a foundation of profit-driven incentives and paternalistic control, it has steadily drifted from its primary mission to heal. The result is a system that creates dependency, punishes dissent, and has fueled an existential crisis in antimicrobial resistance. We can no longer afford to apply superficial fixes to a system that is failing at its core.
The path forward requires a fundamental paradigm shift. We must dismantle the paternalistic, for-profit structures that have corrupted the practice of medicine and replace them with a model centred on patient empowerment, prevention, and partnership. The principles embodied in the Dr Maya framework offer a clear, actionable blueprint. This model directly counters profit-driven corruption by reducing unnecessary consultations; mitigates operational failures by providing accurate, pattern-based triage at scale; and reverses ethical decay by restoring autonomy and informed consent to patients.
This is a call to action for policymakers to regulate predatory economic models, for healthcare leaders to dismantle the systems that punish whistleblowers and perpetuate error, and for patients to demand the agency and knowledge that is rightfully theirs. We must have the courage to abandon failing models and the vision to embrace a future where technology serves humanity, not corporate balance sheets. It is time to champion a system that aims not merely to treat disease but to foster well-being. It is time to rediscover what it means to "heal... not just bodies, but systems."